Cervical Screening
British Sign Language (BSL) signed content: Taking part in NHS cervical screening


Cervical Screening (Smear Tests)
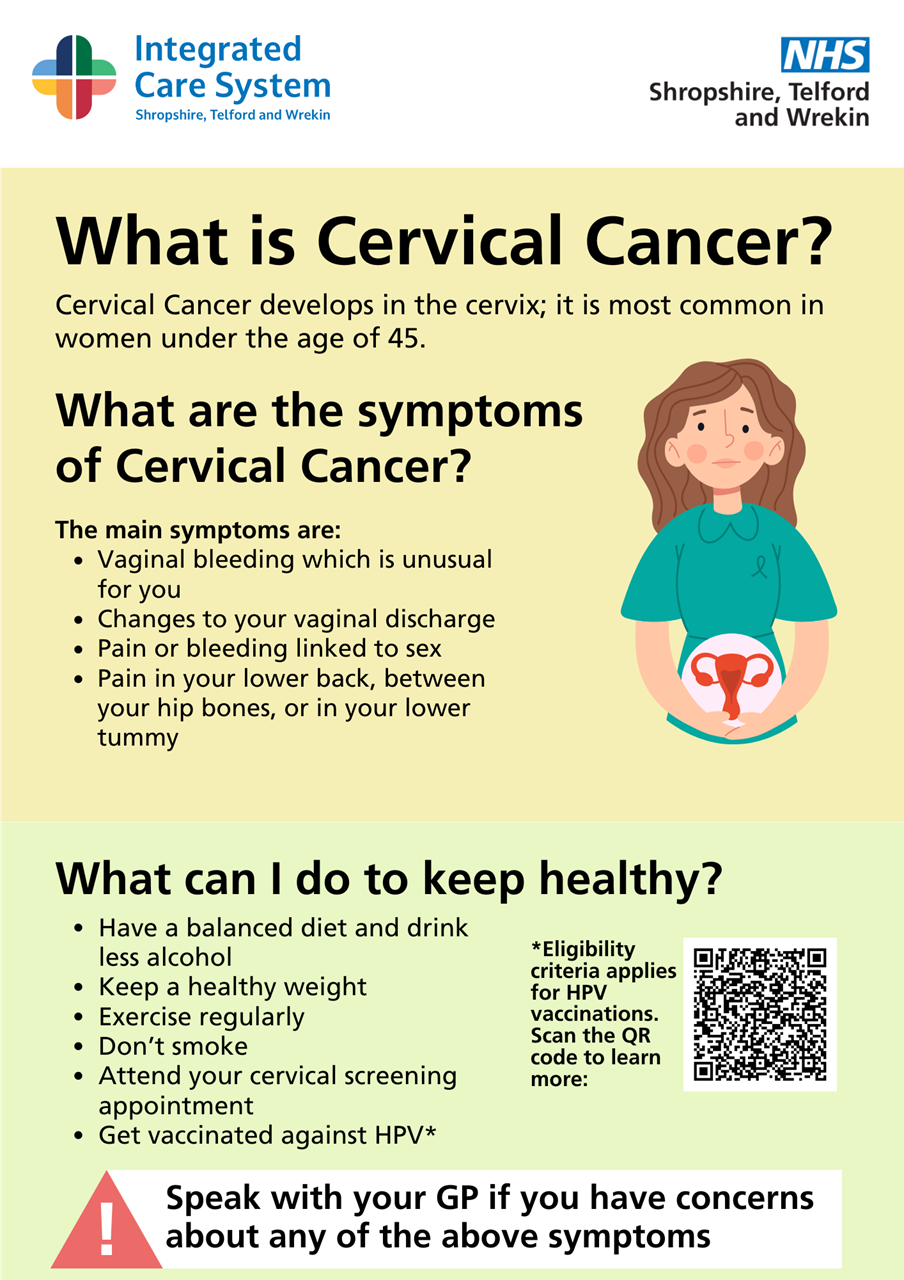
The NHS Cervical Screening Programme saves thousands of lives every year by detecting abnormal cells in the cervix that could develop into cancer, if left untreated.
How often people need to have cervical screening is changing in England from 1st July 2025. Improvements in HPV testing enables the NHS to now offer a more personalised approach to preventing cervical cancer, which means those identified as lower risk won’t need to be screened as frequently, and those at higher risk will continue to be monitored more regularly.
The Human Papillomavirus (HPV) causes nearly all cervical cancers. Since December 2019 all cervical screening samples taken in England have been tested for high-risk HPV. It is a more sensitive and accurate test than the previous method and is the best way to find out who is at higher risk of developing the cell changes that over time could lead to cervical cancer.
At the moment, in England, women and people with a cervix aged 25-49 years are routinely invited for screening every 3 years. Now we have this better test for HPV, the UK National Screening Committee (UKNSC) has recommended that those testing negative, and with no recent history of HPV, won’t need to come for a cervical screening quite so often – every 5 years instead of every 3. If your cervical screening shows you have HPV, you may be invited for more frequent screenings to check HPV has cleared and if not, if any cell changes have developed.
This change is strongly backed by robust scientific evidence. Studies have shown that if a person tests negative for HPV they are extremely unlikely to go on to develop cervical cancer within the next 10 years. Research published by King’s College London showed that 5-yearly screening is as safe as 3-yearly; the same number of cancers will be prevented and less frequent cervical screening tests are needed.
This move brings England into line with Scotland and Wales who have introduced this change, and with women aged 50 – 64 who are already invited every 5 years.
The positive impact of the HPV vaccination is also starting to be seen, with studies in England showing that the HPV vaccine stops 90% of cervical cancer cases. The latest HPV vaccine type introduced in the UK in 2021 is predicted to further reduce cases of women’s cancer and HPV attributable deaths by 16% and 9%, compared to the previous vaccine type.
Even if you've had the HPV vaccination, it's important that you attend your cervical screening. Cervical screening saves lives – so make sure you come forward for your screening when you’re invited, even if it was weeks, months or years ago. If you think you are due but have not yet had an invitation, speak to your GP practice.
HPV Vaccination
Since September 2008 there has been a national programme to vaccinate girls aged 12-13 against human papilloma virus (HPV). There is also a three-year catch up campaign that will offer the HPV vaccine (also known as the cervical cancer jab) to 13 - 18 year old girls.
The programme is delivered largely through secondary schools and consists of three injections that are given over a six-month period. In the UK, more than 1.4 million does have been given since the vaccination programme started.
What is Human Papilloma Virus (HPV)?
Human Papilloma Virus (HPV) is the name of a family of viruses that affect the skin and the moist membranes that line your body, such as those in your cervix, anus, mouth and throat. These membranes are called mucosa.
There are more than 100 different types of HPV viruses, with about 40 types affecting the genital area. These are classed as high risk and low risk.
How Do You Get HPV?
Types of HPV that affect the skin can be passed on by skin contact with an affected person. The types of HPV that affect mouth and throat can be passed on through kissing. Genital HPV is usually spread through intimate, skin to skin contact during sex. You can have the genital HPV virus for years and not have any sign of it.
How HPV Can Cause Cervical Cancer?
Most HPV infections are harmless or cause genital warts, however some types can cause cervical cancer. Most HPV infections clear up by themselves, but in some people the infection can last a long time. HPV infects the cells of the surface of the cervix where it can stay for many years without you knowing.
The HPV virus can damage these cells leading to changes in their appearance. Over time, these changes can develop into cervical cancer. The purpose of cervical screening (testing) is to detect these changes, which if picked up early enough, can be treated to prevent cancer happening. If they are left untreated, cancer can develop and may lead to serious illness and death.
Cancer Research - HPV Facts and Information
NHS - HPV Vaccination - Why, how and when is the vaccination given and what are the side effects
HPV Vaccine- This factsheet is for people who would like information about the human papilloma virus (HPV) vaccine.
1) Booking your appointment
Before you book your appointment, it might help to think about what would make screening easier for you. You might already know what can help or you may want to discuss this with a nurse or health professional who can make some suggestions. Here are some tips that might help:
- If you get anxious sitting in waiting rooms, let the receptionist know. You can ask to book the first appointment of the day, so that you do not have to wait long.
- If you would prefer to be seen by a woman, ask for a female health professional.
- Tell the receptionist if you would like a chaperone. This is a usually another health professional. You might also want a friend, relative or carer present.
- You may feel you need more time for your cervical screening appointment. Ask the receptionist if you can book a longer appointment to give you more time during and after.
You may also wish to consider asking for an appointment just to talk about what happens during the screening first (you do not have to have the test at this appointment).
If you find screening painful a doctor may be able to prescribe creams or medications to help you feel more relaxed.Before your appointment
2) Before your appointment
You may find it helpful to:
- plan your journey
- listen to music or watch something on your phone to help you relax, or bring something to read
- consider what to wear to your appointment; if you feel more comfortable wearing a skirt, dress or long top, it may help you feel more covered (you can keep these clothes on during your test and only take off your underwear)
- speak to the health professional beforehand to discuss your concerns if you think the test may be uncomfortable as they can offer support
- ask someone you trust to go with you, such as a friend, relative or carer/mental health worker, who can also be with you after your appointment
3) Your appointment
- You will have a private space to undress from the waist down and you will have a modesty sheet to cover you – remember you can wear a long top or dress/skirt to help you feel less exposed.
- There may be different positions that could make the test more comfortable for you, like lying on your side. Your healthcare professional will work with you to make sure you are in the most comfortable position.
- A speculum (usually plastic) will be gently put into your vagina. It opens so the health professional can see your cervix. Speculums come in a range of sizes. Talk to your health professional to discuss the size that is most appropriate for you.
- The health professional will use a small, soft brush to take a sample of cells from your cervix.
- Your test could feel uncomfortable but remember, you are in control during the test. It may help to agree a word or hand signal, so the health professional knows to stop immediately if you want them to.
4) Questions to ask the health professional
It might be helpful to think of any questions you want to ask the health professional before your appointment.
We want to make you feel at ease so you have the best possible experience - you can ask for extra support for any reason, including if you:
- have a mental health condition
- take medication that makes you shake
- find it hard to leave your house
- sometimes find it hard to process information
- do not like to feel exposed by removing your clothes
- are embarrassed by showing your body
- have scars
- feel like you might be judged
- feel like a burden
- are afraid it will hurt
- may start to cry or freeze up
- may pass out or faint
- may have a panic attack
- get distressed during a physical examination
- have had a negative cervical screening experience in the past
- have experienced trauma
- are a survivor of sexual violence
- are a survivor of female genital mutilation or cutting (FGM/C)
- want to be warned before the health professional touches you
- find that waiting rooms make your symptoms worse
- find that certain words, actions or positions trigger anxiety attacks or flashbacks
You may want to print out and fill in the extra support checklist to take with you to your screening test. We also have copies of these available at Reception if you wish to complete it before your appointment.
5) After the test
The sample of cells is sent to the laboratory for testing.
We will send your screening result to you by post. The nurse or doctor who does your screening test will tell you when you can expect to get your result letter, and they will also get a copy. Please make sure you tell your GP practice or healthcare professional about any changes to your address.
You may feel anxious while waiting for your results. It may help to speak with someone you trust about how you are feeling.Getting support
6) Getting Support
If you need support, you:
- can talk to a trusted friend, relative or health professional
- may find it helpful to seek spiritual support from a religious or spiritual leader
- may want to talk to someone at Jo’s Cervical Cancer Trust, The Havens, Samaritans or SANEJo’s
Screening Saves Lives Here you can find out about the five national health screening programmes. They can answer any questions or worries you have and can help to make you feel better about going for your cervical screening.
The Eve Appeal is the leading UK national charity funding research and raising awareness into the five gynaecological cancers - womb, ovarian, cervical, vulval and vaginal
The Havens are specialist centres in London for people who have been raped or sexually abused. Telephone 020 3299 6900 for urgent advice or an appointment.
Samaritans is available round the clock, every single day of the year. You can talk to them any time you like, in your own way, about whatever’s getting to you.
Call free, any time: 116 123
Email: jo@samaritans.orgSANE
SANE is a national mental health helpline offering specialist emotional support to anyone affected by mental illness.
SANEline: 0300 304 7000 (every day, 4.30 to 10pm).
Support for victims of sexual violence and abuse
Advice and support for those who are experiencing or feel at risk of sexual violence and abuse is available at: Support for victims of sexual violence and abuse - GOV.UK (www.gov.uk)
National FGM Support Clinics
National FGM Support Clinics (NFGMSCs) are community-based clinics that offer a range of support services for women with female genital mutilation (FGM)
More information and clinic locations can be found at: National FGM Support Clinics - NHS - NHS (www.nhs.uk)
NHS Conditions and Treatments
See the NHS Conditions and Treatments browser for an in-depth description of many common health issues.
Page created: 09 November 2023